Causes and Treatments of Gastrointestinal Bleeding
Gastrointestinal bleeding is a serious medical concern, encompassing several conditions where bleeding occurs within the digestive tract. This complex phenomenon can originate anywhere from the esophagus to the rectum.
It may manifest as overt bleeding with visible symptoms or occult bleeding, which is hidden and often detected through laboratory tests. The causes of gastrointestinal bleeding are diverse, ranging from common conditions such as peptic ulcers, esophageal varices, and gastritis to more complex issues like inflammatory bowel disease and gastrointestinal tumors.
In what follows, we will discuss the intricacies of gastrointestinal bleeding, explain the diverse causes, and discuss the treatment of this important medical challenge.
Causes of GI Bleeding
Gastrointestinal bleeding can be attributed to various conditions affecting the digestive tract’s upper and lower parts.
Upper GI Bleeding
- Peptic Ulcers: Among the leading causes of upper gastrointestinal bleeding, peptic ulcers are erosions that develop in the stomach lining or the upper part of the small intestine. Often triggered by the bacterium Helicobacter pylori or nonsteroidal anti-inflammatory drugs (NSAIDs), peptic ulcers can lead to significant bleeding when left untreated.
- Gastritis: Inflammation of the stomach lining, known as gastritis, can cause bleeding in the upper gastrointestinal tract. Chronic gastritis, frequently linked to Helicobacter pylori infection or prolonged NSAID use, can erode the mucosal lining, resulting in bleeding.
- Esophageal Varices: Commonly associated with liver cirrhosis, esophageal varices are enlarged, fragile veins in the esophagus. Increased pressure within these veins can lead to rupture, causing severe upper GI bleeding, which is a medical emergency.
- Mallory-Weiss Tears: Tears in the mucous membrane where the esophagus meets the stomach, known as Mallory-Weiss tears, can occur due to severe vomiting, retching, or other forms of increased abdominal pressure, leading to upper GI bleeding.
Lower GI Bleeding
- Diverticulosis: The development of small pouches, or diverticula, in the walls of the colon characterizes diverticulosis. Bleeding can occur if these pouches become inflamed or rupture, leading to lower GI bleeding.
- Colitis: Inflammation of the colon, encompassing infectious, ischemic, and inflammatory bowel diseases such as Crohn’s disease and ulcerative colitis, can result in bleeding. Chronic inflammation weakens the mucosal lining, making it susceptible to bleeding.
- Anorectal Disorders: Conditions affecting the anus and rectum, including hemorrhoids and fissures, can cause bleeding in the lower gastrointestinal tract. Although usually not life-threatening, these disorders can lead to discomfort and recurrent bleeding.
- Polyps and Colorectal Cancer: Abnormal growths in the colon, such as polyps, can bleed and may progress to significant blood loss. Colorectal cancer can also manifest with bleeding as a prominent symptom.
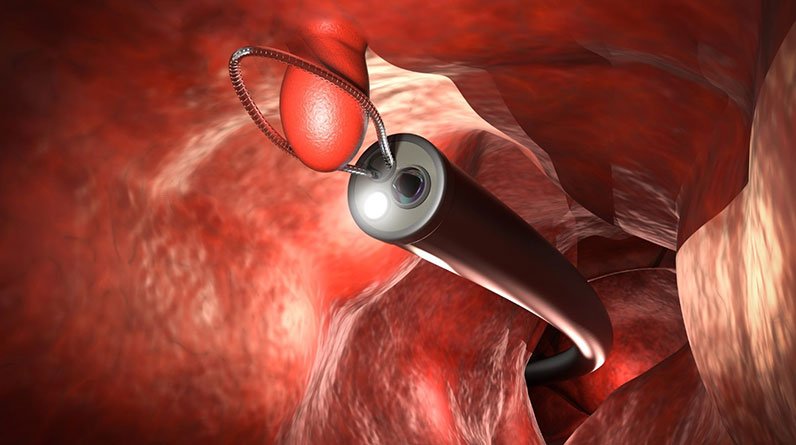
Treating GI Bleeds
(NOTE: This is a DEMO website, and portions of the content will be blurred. The full un-blurred content will be provided to license holders).
Maintaining a balanced and healthful diet, avoiding excessive alcohol and tobacco consumption, and managing chronic conditions effectively will contribute to overall gastrointestinal well-being.
Lifestyle choices, coupled with early detection and appropriate treatment of underlying gastrointestinal conditions, form a proactive strategy to safeguard against the potential complications of gastrointestinal bleeding.
