Diabetes and Kidney Health
Diabetes, a chronic metabolic condition characterized by elevated blood glucose levels, has profound implications for kidney function. The dangerous interplay between diabetes and the kidneys is important to understand in the maintenance of kidney health.
Diabetes is broadly categorized into two types: Type 1, an autoimmune condition where the pancreas fails to produce sufficient insulin, and Type 2, characterized by insulin resistance and insufficient insulin production.
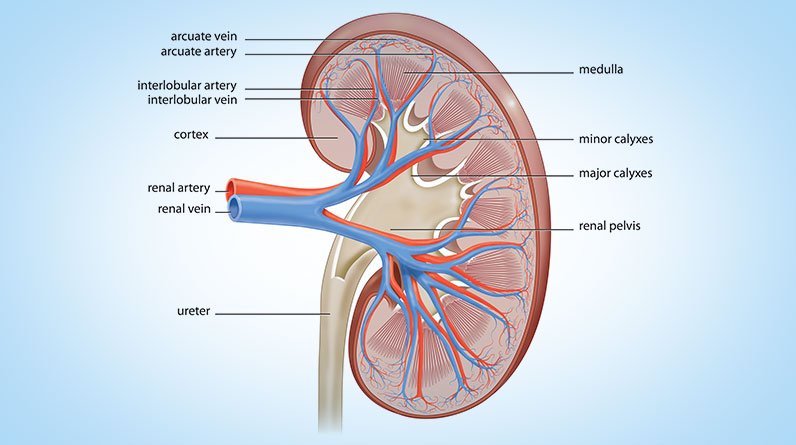
The kidneys play a pivotal role in maintaining the body’s internal balance by filtering blood and eliminating waste products through the urinary system. However, in the context of diabetes, prolonged exposure to high blood glucose levels can lead to complications that detrimentally affect kidney function.
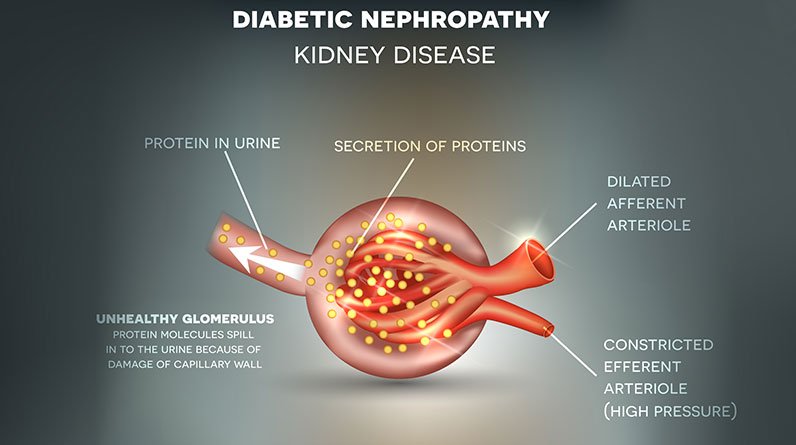
- Glomerular Damage: The glomeruli, tiny filtering units within the kidneys responsible for filtration, are particularly vulnerable. Persistent high blood sugar damages the delicate filtering units, leading to a condition known as diabetic nephropathy.
- Increased Pressure: Diabetes often coincides with hypertension, further exacerbating the strain on the kidneys.
- Proteinuria: In diabetes-related kidney damage, there is an increased permeability of the glomerular filtration barrier. This allows proteins, normally retained in the bloodstream, to leak into the urine – a condition known as proteinuria.
Diabetic nephropathy, a specific manifestation of kidney damage in individuals with diabetes, is a progressive condition that evolves over years. The early stages are characterized by small amounts of protein in the urine, known as microalbuminuria. This can be detected by a urine test.
As the condition advances, it may escalate to macroalbuminuria, where larger amounts of protein are excreted in the urine. Left untreated, diabetic nephropathy can lead to chronic kidney disease (CKD) and can also lead to end-stage renal disease (ESRD), necessitating dialysis or kidney transplantation.
Individuals with diabetes must learn that they are at high risk of developing impaired kidney function if their diabetes is poorly controlled.
Symptoms, Complications, and Risks
Recognizing early signs of kidney problems in individuals with diabetes is crucial for timely intervention. Common symptoms include changes in urination, swelling, fatigue, and elevated blood pressure.
Diabetes-related kidney damage can progress to severe complications beyond the aforementioned symptoms. These include diabetic nephropathy, fluid retention, cardiovascular disease, and electrolyte imbalances.
- Diabetic Nephropathy: This condition, characterized by damage to the glomeruli, is a common complication that can lead to proteinuria, hypertension, and declining kidney function. Most notably, diabetes significantly increases the risk of chronic kidney disease (CKD) and eventual kidney failure. Several factors contribute to this heightened risk including:
- Prolonged High Blood Sugar Levels: Persistent hyperglycemia places stress on the kidneys, leading to structural changes and impairing their filtering function.
- Hypertension: High blood pressure, prevalent in diabetes, is a major contributor to kidney damage. The kidneys play a crucial role in blood pressure regulation, and dysfunction in this process can exacerbate hypertension.
- Genetic Factors: Some individuals with diabetes may have a genetic predisposition to kidney problems, further elevating their risk of CKD.
- Poorly Managed Diabetes: Inadequate glycemic control, coupled with suboptimal blood pressure management, increases the likelihood of kidney complications.
Understanding the intricate web of symptoms, complications, and risks associated with kidney problems in diabetes underscores the importance of proactive healthcare.
Treatment and Management of Diabetes
Managing diabetes effectively is not only crucial for glycemic control but also plays a pivotal role in safeguarding kidney health.
The intricate relationship between diabetes and kidney function necessitates a comprehensive approach that encompasses lifestyle modifications, medical interventions, and preventative strategies.
(NOTE: This is a DEMO website, and portions of the content will be blurred. The full un-blurred content will be provided to license holders).